
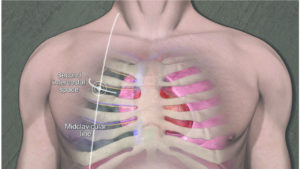
The following image (of a different casualty) shows the common location that a chest tube is inserted. The tube sits in between the inside of the chest wall and the damaged lung and is attached to a one-way valve system allowing drainage out of the chest only. With changes in chest pressure during breathing, blood and air from around the damaged lung are pushed through the chest tube and out through the one-way valve system into a collecting reservoir, gradually allowing the lung to re-inflate.

Once the casualty in the case study’s surgery was complete, she was medically evacuated to a higher-level hospital facility to complete her recovery.
Fortunately for the casualty, her wound was relatively minor, however chest trauma, both blunt and penetrating, can rapidly lead to death under certain circumstances if the first-responder doesn’t identify and treat particular life-threatening conditions.
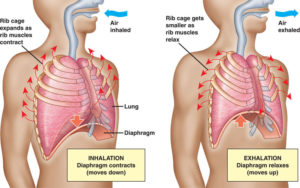
To understand these conditions it’s important to have a basic understanding of how breathing works, and the pressures generated in the chest during inspiration and expiration. There are many muscles involved in breathing, but the key one is the diaphragm, which is the large flat muscle at the bottom of the chest cavity that acts like the plunger of a syringe to draw air into the lungs with inspiration and push air back out of the lungs on expiration. When the diaphragm contracts and moves down, negative pressure is created in the chest and air is sucked into the lungs through the airway. When the diaphragm relaxes and moves back up to its resting position, positive pressure is created inside the chest, which pushes the air back out of the lungs through the airway.
This mechanism works well as long as the system is not damaged, with both lungs inflated, and only one hole for air to come in and out of the chest – being the airway. A fine layer of fluid between the outside of the lungs and the inside of the chest wall causes the lung to adhere slightly to the inner chest wall and prevents the lungs from collapsing on full expiration.
In the case study above, where a penetrating injury has caused a hole in the side of the chest cavity and damaged the underlying lung, a few things occur to disrupt the normal breathing mechanism. First, the adhesion between the lung and the inside of the chest wall is lost by entry of air into that space and the lung collapses down like a popped balloon, in a condition known as pneumothorax. This collapse can be partial or complete in the damaged lung, with the immediate effect on the casualty being a reduction in the lung volume available to get oxygen into their system. Fortunately the human body has an amazing amount of redundancy and can function quite well on one lung, as seen in the case study above. Pneumothorax is often seen in the civilian trauma context following blunt trauma such as a car crash, where injuries such as broken ribs can internally puncture the lung and cause it to collapse.
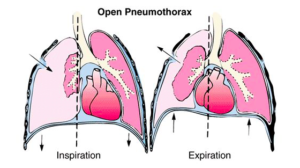
A second, and more imminent, concern in a penetrating chest injury is the concept of a “sucking” chest wound, or an open pneumothorax. In this setting a hole has been made in the side of the chest wall, which if it is big enough (roughly 2/3 the size of the trachea or wind pipe), air will move in and out of that hole as opposed to moving in and out of the airway. This occurs due to air wanting to move along the path of least resistance, and if a hole in the side of the chest offers less resistance than the airway, when the diaphragm contracts and creates negative pressure in the chest, this pressure will equalize through the hole in the side of the chest. The end result is that air is only moving in and out of the chest through the hole made by the injury, and ends up around the damaged lung, with little or no air getting into the undamaged lung. If left untreated this situation will lead to the casualty getting insufficient movement of air into their lungs, and hence insufficient oxygen into their system, leading to eventual death.
The following video graphically illustrates a sucking chest wound.
https://www.youtube.com/watch?v=vL9Kyf6-pd0
The simple life-saving initial management of a sucking chest wound is to cover it. Even though the lung underlying the hole in the chest wall will remain deflated, by covering the hole in the chest and preventing air from being able to get in through it to equalize the chest pressure on inspiration, air will once again be drawn in through the airway and into the good lung. As in the case study above, the casualty can then be taken to hospital where their chest wounds can be properly managed and a chest tube can be inserted.
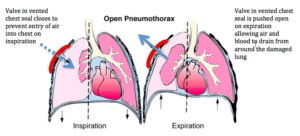
The first-responder can use any manner of things to close a sucking chest wound, ranging from a gloved hand, to pulling the overlying muscle and skin tissues over the hole, to purpose-designed or improvised occlusive dressings. In the military context, we used to find that a product known as Hydrogel worked well. Used traditionally for attaching demolition charges to all manner of surfaces by our breaching brethren, Hydrogel proved outstanding at sticking to hairy, sweaty, dirty, and bleeding soldier’s chests on the battlefield. Modern day purpose-designed chest seals have adopted this gel adhesive to good effect. Another feature of the new generation commercial chest seals is the addition of a one-way valve, which acts in the same manner as the chest drain described above.



Recent evidence has shown that the addition of a vent in an occlusive chest seal significantly reduces the likelihood of another life-threatening chest condition known as a tension pneumothorax (Butler 2013; Kheirabadi 2013; Kotora 2013).
The final life-threatening chest injury that I will discuss in this article, and in my opinion the most important for a first-responder to be aware of, is tension pneumothorax. Tension pneumothorax occurs when air leaking internally from a damaged lung accumulates between the inside of the chest wall and the damaged lung, gradually building up pressure with every breath until the amount of air trapped in one side of the chest starts to push on the heart and the undamaged lung. Left untreated, the pressure from this trapped air will collapse the undamaged lung and kink off the major blood vessels to and from the heart, leading to a situation where the casualty cannot breathe and has minimal output from their heart, eventually causing death. Anyone who has seen the classic film “Three Kings” will have seen a graphic representation of tension pneumothorax after Mark Wahlberg’s character gets shot through the chest. The scene is actually a decent depiction the “air hunger” and anxiety that a casualty with a tension pneumothorax displays as pressure accumulates. In the scene George Clooney puts his ER skills to good use by correctly diagnosing and treating the tension with a procedure known as needle thoracocentesis (Ice Cube doesn’t add any real value!).
A slightly more reputable video of the procedure is presented here for anyone interested.
The typical injury causing a tension pneumothorax is a small penetrating chest injury such as those seen from ball bearings or shrapnel in IEDs, or gunshot wounds. Unlike in open pneumothorax, the hole left in the chest wall from a small penetrating missile will either seal itself, or if it does remain open, will not be large enough for air to preferentially move in and out of it rather than the airway. For that reason air continues to enter through the airway as usual, passes into the damaged lung on inspiration, and then a small amount leaks through the hole in the damaged lung and gets trapped between that lung and the inside of the chest wall. This process repeats with every inspiration and the casualty gets increasingly short of breath and anxious, until they will eventually lose consciousness and die if untreated.
Whilst tension pneumothorax is more often seen in penetrating chest injuries, it can certainly be seen following blunt, or other forms of chest trauma including dive injuries. Tension pneumothorax can also occur after a sucking chest wound has been treated with an occlusive dressing, or if a vented seal has been used and the vent has become clogged with dried blood. In that setting it is reasonable to peel the dressing back and see if pressure vents from the wound in the chest, before resealing the wound or decompressing the chest with a needle if the tension remains unresolved. Furthermore, for anyone who does aeromedical evacuation, any patient with a pneumothorax on the ground must be monitored closely when taken to altitude, especially in unpressurised aircraft. As the casualty gains altitude, any trapped gas inside their body will expand due to reduced atmospheric pressure. If gas is trapped within the chest cavity, as in pneumothorax, then as it expands it can cause tension. If the situation allows, it is ideal to place chest tubes in casualties with a suspected pneumothorax before aviation medical evacuation (AME), however if you’ve got to get back in the air quickly then have the needle at the ready!
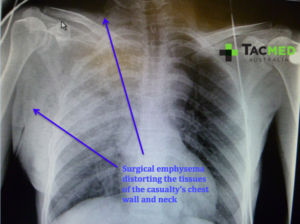
The following X-rays show the normal chest anatomy labeled in the first image, and a tension pneumothorax seen in the second image. The distortion of the anatomy caused by the pressurised air can be seen and it can be appreciated that air entry into the undamaged lung will be reduced, and blood flow to and from the heart will be compromised. Those in the medical profession will recognise this second X-ray as “the X-ray that should never be taken” meaning that the condition should ideally have been recognized clinically and treated without burning time getting an X-ray done.
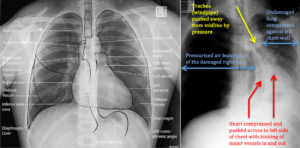
When looking at the X-ray of the tension pneumothorax above, it can be seen that the insertion of a needle into the appropriate space (being the second intercostal space, mid-clavicular line – illustrated below) will enter into the area of pressurised air and vent it. If the diagnosis is correct, a rush of air will escape from the needle and the casualty’s clinical condition will improve almost instantly. The patient will still require a chest tube, and the tension may re-accumulate if the needle blocks or becomes kinked however the initial life-saving management is the timely insertion of the needle.
So there it is, a quick run down of pneumothorax, open pneumothorax and tension pneumothorax. Naturally there’s a whole range of other chest injuries not covered by this article that a first-responder should be aware of, but these three are a good start.
The take home points for the first-responder are to rapidly occlude any sucking chest wounds and to keep a sharp eye out for tension pneumothorax in anyone with chest, or even abdominal injuries, who has increasing shortness of breath and deteriorating vital signs. For those among the audience who go in harm’s way, the take home point is to never be tempted to remove the Kevlar from your chest rig, no matter how low-profile the job, or how many kilos of other equipment you need to carry. That plate might just be the difference between having a good story to tell over a beer, or someone like me sticking needles and tubes in your chest!
Thanks for reading, as always questions and comments are welcome.
Kind regards, Dan.
References:
Butler, F, Dubose, JJ, Otten, EJ, Bennett, DR, et al. 2013, ‘Management of open pneumothorax in Tactical Combat Casualty Care: TCCC Guidelines change 13-02’, Journal of Special Operations Medicine, vol. Fall, no. 13, pp. 81-86.
Kheirabadi, B, Terrazas, IB, Koller, A, Allen, PB, et al. 2013, ‘Vented versus unvented chest seals for treatment of pneumothorax and prevention of tension pneumothorax in a swine model’, Journal of Acute Care Surgery, vol. 75, no. 1, pp. 150-156.
Kotora, J, Henao, J, Littlejohn, LF, Kircher, S 2013, ‘Vented chest seals for prevention of tension pneumothorax in a communicating pneumothorax’, Journal of Emergency Medicine, vol. 45, no. 5, pp. 686-694.












COMMENTS